Cognitive Behavioral Therapy
|
What is Cognitive Behavioral Therapy?
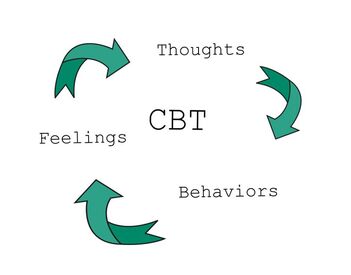
Cognitive Behavioral Therapy, otherwise known as CBT, is an evidence-based treatment for a variety of mental health disorders in which cognitive and behavioral shifts contribute to changes in emotions. This treatment is evidence-based because an abundance of research has demonstrated that engagement in CBT results in symptom reduction or elimination of a variety of psychological difficulties (as cited in Chand et al., 2023). What does this evidence-based treatment entail? CBT aims to address maladaptive cognitions and behaviors via skill-based interventions that assist with challenging those unhelpful thoughts and behaviors. Cognitive behavioral therapy is generally a more structured and directive treatment approach. In other words, CBT will incorporate specific treatment planning so you know what to expect. Often, an agenda will be set at the beginning of each session and homework will be assigned each week, which may consist of worksheets or planned behavioral assignments. The goal of CBT will be for you to develop tools for managing difficulties during and after treatment. Some treatment may be manualized, meaning the provider will use a manual created by experts and supported by research to guide treatment. Cognitive behavioral therapy also often includes objective symptom monitoring in which self-report measures are completed to track symptoms and ensure that you are benefiting from your treatment. |
|
What exactly does this treatment consist of?
First, each session typically will start with setting an agenda. That may include discussing a stressor, learning a new thought challenging skill, completing a worksheet, or determining a specified homework assignment. Because CBT emphasizes skills based interventions, homework is typically required to assist with developing and applying the skills learned in treatment. For instance, if your provider encourages evaluating thinking patterns in a more scientific way, your provider may give you a handout to read on maladaptive thinking patterns and a corresponding worksheet to complete to start actively and scientifically challenging thoughts. If, for example, a patient is having what are called cognitive distortions, or distorted, unhelpful, and often unkind thoughts based on biases from one’s past, the therapist may ask that the patient identify one thought every day that may or may not be accurate (Gilson et al., 2009). The therapist may also suggest looking for evidence for and against that thought. |
One common cognitive distortion we see when someone is struggling with an anxiety disorder is called catastrophizing. If someone is catastrophizing, they may often have the automatic thought of “I can’t handle this.” To challenge this thought, a clinician may suggest looking for evidence for and against this thought, asking you questions like, have you ever ‘handled’ this before and if so, how? If you have not handled the situation before, the therapist may ask you what evidence you have that you would not be able to handle if the catastrophe became a reality.
Behavior modification often requires additional assignments, such as behavioral/ activity tracking and planning in addition to implementing alternative behaviors. In depression treatment, for example, structured activity planning is critical. Why? Because avolition, or loss of motivation, is a common symptom of depression. Many people struggling with depression are hoping that, one day, they will wake up motivated to do what they do not feel like doing. In opposition to this, in what is called, behavior activation, the patient will identify activities that feel rewarding or helpful to increase motivation (Gilson et al., 2009). It will be emphasized that action/ behavior comes before emotional shifts; in other words, we must do something that makes us happy in order to start feeling happy (Gilson et al., 2009). In CBT treatment for anxiety disorder, the behavioral assignments will likely be in the form of exposure work; your therapist will ask you to slowly and systematically start doing things that make you uncomfortable or anxious so that you can overcome those fears.
In sum, the goal of CBT is to help you take control of your thinking and behaving in order to feel better. The highly effective CBT skills will help you to do so both in and out of treatment.
References
Chand, S.P., Kuckel, D. P., & Huecker, M. R. (2023), Cognitive behavior therapy. StatPearls Publishing LLC. https://www.ncbi.nlm.nih.gov/books/NBK470241/
Gilson, M., Freeman, A., Yates, M. J., & Freeman, S. M. (2009). Overcoming depression: A cognitive therapy approach: Therapist Guide. (Illustrated ed.) Oxford University Press.
Behavior modification often requires additional assignments, such as behavioral/ activity tracking and planning in addition to implementing alternative behaviors. In depression treatment, for example, structured activity planning is critical. Why? Because avolition, or loss of motivation, is a common symptom of depression. Many people struggling with depression are hoping that, one day, they will wake up motivated to do what they do not feel like doing. In opposition to this, in what is called, behavior activation, the patient will identify activities that feel rewarding or helpful to increase motivation (Gilson et al., 2009). It will be emphasized that action/ behavior comes before emotional shifts; in other words, we must do something that makes us happy in order to start feeling happy (Gilson et al., 2009). In CBT treatment for anxiety disorder, the behavioral assignments will likely be in the form of exposure work; your therapist will ask you to slowly and systematically start doing things that make you uncomfortable or anxious so that you can overcome those fears.
In sum, the goal of CBT is to help you take control of your thinking and behaving in order to feel better. The highly effective CBT skills will help you to do so both in and out of treatment.
References
Chand, S.P., Kuckel, D. P., & Huecker, M. R. (2023), Cognitive behavior therapy. StatPearls Publishing LLC. https://www.ncbi.nlm.nih.gov/books/NBK470241/
Gilson, M., Freeman, A., Yates, M. J., & Freeman, S. M. (2009). Overcoming depression: A cognitive therapy approach: Therapist Guide. (Illustrated ed.) Oxford University Press.